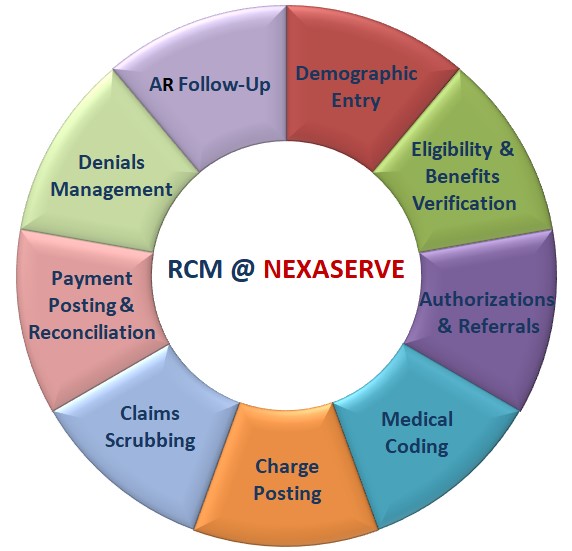
Demographic Entry
We accurately capture and input all essential patient information into the system to establish the foundation for smooth billing.
Includes:
• Patient personal details (Name, DOB, Contact, etc.)
• Insurance details (Payer, Plan Type, Policy ID, etc.)

Eligibility & Benefits Verification
Before services are rendered, we verify the patient's insurance coverage and benefits to prevent claim rejections and reduce patient payment delays.
Our verification covers:
• Policy status
• Covered services
• Co-pays, deductibles, and out-of-pocket limits
Authorizations & Referrals
We proactively obtain necessary authorizations from insurance companies and referrals from referring physicians to ensure compliance and prevent denials.
Services include:
• Pre-certification requests
• Referral documentation tracking
• Follow-up on pending approvals

Medical Coding
Certified coders translate clinical documentation into accurate CPT and ICD-10 codes for procedures and diagnoses.
We ensure:
• Compliance with payer guidelines
• Proper code assignment from HPI and treatment plan
• Maximized reimbursement with minimized risk

Charge Posting
We meticulously post all charges into your billing system, ensuring alignment with coding, authorizations, and patient demographics.
Our process includes:
• Accurate entry of CPT/ICD codes
• Verification of charge amounts
• Inclusion of insurance and authorization data
Claims Scrubbing
We review claims for errors and inconsistencies before submission to ensure clean claims and reduce denials.
Our process includes:
• Accurate entry of CPT/ICD codes
• Verification of charge amounts
• Inclusion of insurance and authorization data

Payment Posting & Reconciliation
We post insurance and patient payments promptly and reconcile payments against Explanation of Benefits (EOBs) to maintain financial accuracy.
Our services include:
• Electronic and manual payment posting
• Adjustment entries
• Daily and monthly reconciliation

Denials Management
Our team analyzes and resolves claim denials efficiently to recover revenue and minimize write-offs.
Includes:
• Root cause identification
• Appeal preparation and submission
• Corrected claim resubmissions

Accounts Receivable (A/R) Follow-Up
We actively follow up with both insurance payers and patients to ensure timely claim resolution and payment collection.
Activities involve:
• Insurance claim status checks
• Patient balance outreach
• Aging report management